I remember the first time I worried about my energy fading with age. Small tasks took longer, and my curiosity about biological age grew into a search for practical answers.
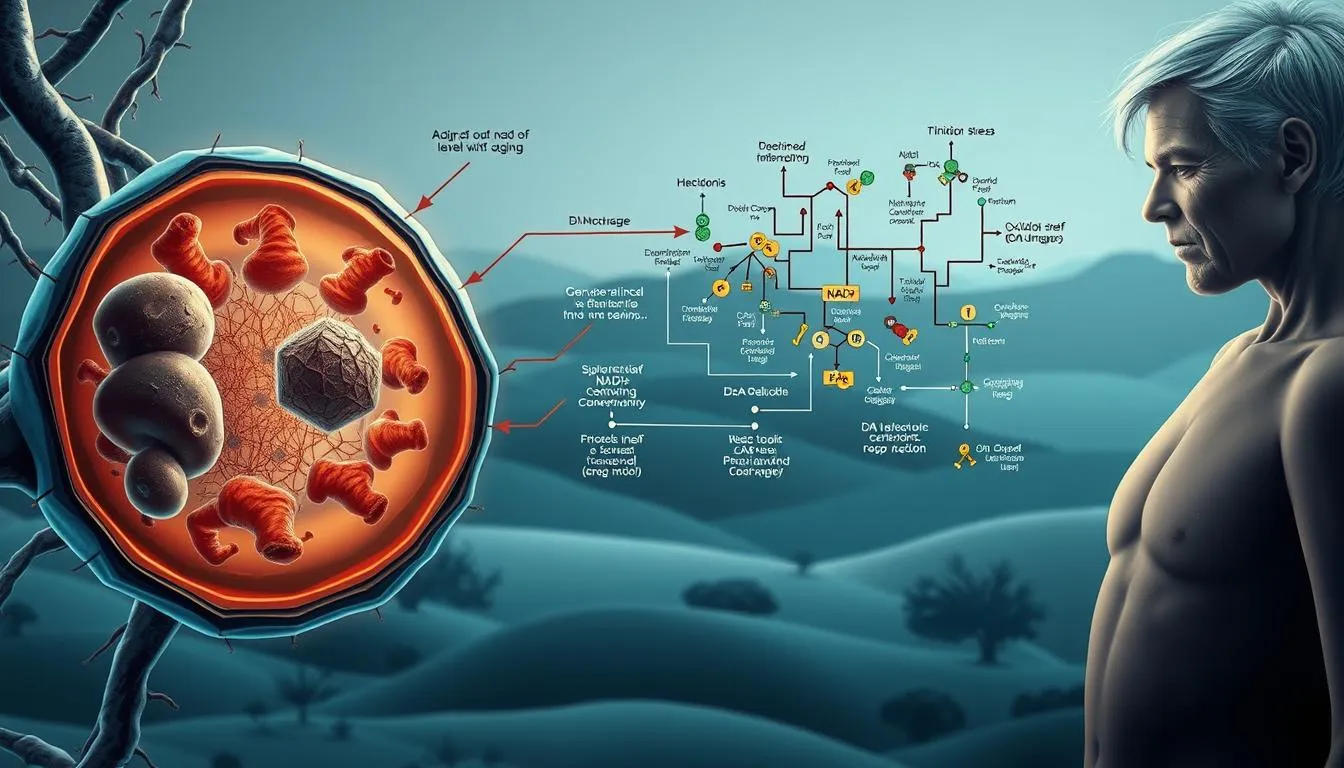
Scientists link these changes to drops in nicotinamide adenine dinucleotide across tissues. That decline nad with aging can affect cellular repair and energy, so many older adults look for ways to support nad levels. For comprehensive aging strategies, explore longevity lifestyle optimization and consider sustainable supplement sourcing practices.
This guide explains how oral supplementation with precursors such as nicotinamide riboside and nicotinamide mononucleotide may change blood markers, blood pressure, and tissues like skeletal muscle and the liver.
Evidence so far shows modest, variable benefits. Trials differ in dose and duration, and many are small.
My aim is to walk you through the core biology, what the studies say about fatty liver disease and other liver disease signals, safety, and how to judge claims using tools like google scholar.
Key Takeaways
- Age-related decline in adenine dinucleotide matters for energy and repair.
- Oral supplementation can raise nad levels modestly in blood and some tissues.
- Most human trials show small, variable effects on blood pressure and inflammation.
- Nicotinamide riboside and nicotinamide mononucleotide are the main studied options.
- Evidence on fatty liver and long-term outcomes is still emerging.
- Use google scholar to check primary research and study quality.
What Are NAD+ Supplements? A friendly overview for today’s reader
Nicotinamide adenine dinucleotide is a small molecule your cells use to turn food into energy. It also powers enzymes that repair DNA and help cells cope with stress.
Common precursor forms include nicotinamide riboside and nicotinamide mononucleotide. These precursors are studied for oral supplementation so cells can support nad metabolism and, in some trials, increase nad in blood and tissues.
The role nad plays goes beyond energy. It drives signaling through sirtuins and PARPs, which is why researchers look at exercise recovery, brain support, and heart health.
Cells mostly rebuild this molecule via the salvage pathway, converting precursors into usable adenine dinucleotide. Responses vary by tissue — whole-blood changes are more consistent than skeletal muscle gains in many studies.
Trials differ in dose, duration, and measurement methods, so results are mixed. Expect subtle, incremental benefits rather than dramatic shifts.
- Generally well tolerated in healthy middle-aged people and older adults.
- Study variability means more research is needed for clear clinical outcomes.
- To read original research, search titles and authors on google scholar for primary trials and reviews.
| Feature | What to expect | Notes |
|---|---|---|
| Form | nicotinamide riboside, nicotinamide mononucleotide | Oral supplementation targets the salvage pathway |
| Common results | Modest increase in whole-blood levels | Tissue responses vary (blood vs skeletal muscle) |
| Tolerability | Generally well tolerated | Most trials report few adverse effects in older adults |
| Research tip | Check primary trials on google scholar | Look for dose, duration, and assay methods |
Inside NAD+ biology: how nicotinamide adenine dinucleotide powers cellular health
Understanding how cells make and use nicotinamide adenine dinucleotide explains why energy and repair fade with age.
Redox, ATP, and the role of nicotinamide adenine in metabolism
Nicotinamide adenine acts as an electron carrier in redox reactions that drive ATP production. Electrons move from food-derived molecules to the respiratory chain via this adenine dinucleotide, allowing mitochondria to make energy.
When redox balance shifts, cells face higher oxidative stress, and energy output falls. That link explains why maintaining adequate nad levels matters for metabolic health and tissues like skeletal muscle.
Sirtuins, PARPs, and NAD+ as a signaling co-substrate
This molecule is also consumed by sirtuins and PARP1 as a co-substrate. Those enzymes connect energy status to gene regulation and DNA repair.
Higher PARP or CD38 activity raises demand, which can reduce pools available for sirtuin activity. Cell Rep. papers often map how these shifts affect chromatin remodeling and cell rep.
NAD metabolism, biosynthesis, and the salvage pathway
Cells build nicotinamide adenine via de novo routes and recycling. The salvage pathway drives most nad biosynthesis in adults.
Nicotinamide phosphoribosyltransferase (NAMPT) is rate-limiting for recycling nicotinamide back into usable forms. Low NAMPT or high consumption makes maintaining nad levels harder with age.
Common nad precursors (NR, NMN, NAM) feed the salvage route. Changes in supply and demand both matter, so read methods in primary studies on google scholar for assay details.
| Function | Mechanism | Key enzyme | Tissue note |
|---|---|---|---|
| Energy production | Electron shuttle for oxidative phosphorylation | Mitochondrial dehydrogenases | Skeletal muscle shows variable increases vs blood |
| DNA repair & gene regulation | Co-substrate for PARPs and sirtuins | PARP1, SIRT family | High consumption lowers available pools |
| Recycling | Salvage pathway for nad synthesis | NAMPT | Rate-limiting for tissue-specific maintenance |
Why NAD+ levels decline with age: hallmarks, inflammation, and DNA damage
As we age, two opposing forces — higher consumption and poorer recycling — drive steady falls in cellular adenine dinucleotide.
“Inflammaging” means chronic, low-grade inflammation that slowly shifts tissue metabolism. Immune signals raise CD38 activity, an enzyme that consumes this cofactor. Over time, this contributes to a noticeable decline nad across organs.
Accumulated dna damage triggers PARP1 to repair breaks. That is helpful short-term, but frequent activation becomes a major drain on nicotinamide adenine reserves.
Recycling bottlenecks: NAMPT and NNMT
Levels of nicotinamide phosphoribosyltransferase tend to fall with age. That enzyme limits the salvage route and slows nad biosynthesis, so cells rebuild cofactors less efficiently.
At the same time, NNMT methylates nicotinamide and diverts it from the salvage path. This methylation lowers net nad metabolism and tightens the supply side.
| Driver | Effect on cofactor pools | Consequence | Notes |
|---|---|---|---|
| Inflammaging / CD38 | Increased consumption | Lower steady-state levels | Common in immune-rich tissues |
| DNA repair / PARP1 | Acute high demand | Transient depletion with repeated damage | Linked to genomic instability |
| NAMPT decline & NNMT activity | Reduced recycling and diversion | Bottleneck in biosynthesis | Affects tissue variability and resilience |
These pressures explain links to aging hallmarks like impaired proteostasis and altered intercellular communication. Human studies show tissue-specific drops; some compartments fall faster under stress or disease.
Practical tip: Inspect pathway diagrams and original figures on google scholar to see enzyme maps and quantify effects. These mechanistic clues also guide multitarget strategies beyond single precursors, which we revisit later.
Preclinical evidence at a glance: what animal models tell us about boosting NAD+
Preclinical work gives clear, actionable signals about biological effects and mechanisms. Rodent studies are the backbone of hypotheses now moving into human trials.
Muscle, mitochondria, and stress
Robust in vivo nad experiments show improved muscle function and endurance after restoring cofactor pools. Many reports link gains to mitochondrial biogenesis and reduced oxidative stress.
Cardiometabolic, organ, and cognitive signals
Mouse work commonly reports better glucose tolerance and cardiovascular performance. Liver, heart, and kidney models show greater resilience after injury.
Preclinical alzheimer disease models also show improved memory and nerve repair, suggesting neuroprotection in some settings.
Stem cells and mechanisms
Elevated levels improve stem cell quality—especially muscle and hematopoietic compartments—boosting repair capacity. Mechanistic drivers include stronger sirtuin signaling, lower inflammation, and better DNA repair support.
Takeaway: Animal results give a strong rationale for human testing, but dosing, bioavailability, and timing differ across species. Scan key studies on google scholar to check doses, endpoints, and methods. Repeat searches on google scholar to follow emerging trials that test nad metabolism hypotheses in people.
Human clinical evidence: what we know right now
Human trials now show how oral precursors shift biochemical markers in people across middle and later life. Studies focus on blood signals, vascular tests, and short-term immune readouts rather than long-term outcomes.
Healthy, middle-aged, and older adults: changes in nad levels and safety
Multiple trials report that oral supplementation with nicotinamide riboside supplementation or nicotinamide mononucleotide can raise whole-blood and PBMC nad levels. For example, NR at 500 mg twice daily for six weeks increased PBMC levels ~60% and NAAD about sevenfold.
Safety: Doses from 300–1,000 mg/day show good tolerability with few adverse effects across middle-aged older volunteers.
Cardiovascular markers: blood pressure and arterial stiffness signals
One trial found exploratory reductions in systolic blood pressure and arterial stiffness after riboside supplementation, but those signals did not survive multiple-comparison correction. Other studies saw no change in blood pressure, so larger samples are needed.
Inflammation and biological age proxies
Short-term trials in older adults reported large drops (≈50–70%) in cytokines such as IL-6, IL-5, and IL-2 without increases in human skeletal muscle levels. Muscle nad changes remain inconsistent across studies.
| Endpoint | Typical result | Note |
|---|---|---|
| Whole-blood / PBMC | Increase nad levels | Consistent dose-response (300–1,000 mg/day) |
| Blood pressure | Mixed / exploratory | One trial signal, not definitive |
| Inflammation | Marked cytokine drops in older adults | Short-term immune modulation observed |
Practical takeaways: Oral regimens can boost nad markers and may influence inflammation and vascular metrics, but robust clinical outcomes are still pending. Track new trials in npj aging and verify protocols and results on google scholar for the latest evidence. For deeper searches, check google scholar clinical trial reports and follow-up papers on dose, duration, and tissue-specific uptake.
Nicotinamide riboside (NR): dosing, outcomes, and open questions
When researchers test nicotinamide riboside in humans, results depend heavily on dose, time, and the tissue measured.
Common dosing ranges from 100 to 2,000 mg/day. Oral supplementation at 500 mg twice daily for six weeks raised PBMC markers ~60% in a crossover trial and showed exploratory drops in systolic blood pressure and arterial stiffness.
Whole-blood increases are the most consistent signal, while rises in skeletal muscle are unreliable. Short trials (7 days) often did not change muscle mitochondrial function or sirt1 activity despite higher circulating levels.
Metabolic outcomes are mixed. Some small studies report minor fat loss and higher sleeping energy expenditure. Others show no change in insulin sensitivity or mitochondrial respiration in overweight adults.
Safety and variability: NR is generally well tolerated in older adults with few adverse events. Outcomes vary by baseline health, dose, duration, and analytic methods.
| Dose range | Typical biochemical change | Clinical signal |
|---|---|---|
| 100–2,000 mg/day | Blood/PBMC nad levels rise | Mixed effects on fat mass and blood pressure |
| Short (7 days) vs weeks | Fast blood gains, slow tissue uptake | Sirt1 activity often unchanged in muscle |
Open questions: What is the optimal dose and who benefits most? Compare trials side-by-side on google scholar to judge methods, endpoints, and real-world relevance.
Nicotinamide mononucleotide (NMN): what clinical trials are reporting
Clinical trials testing nicotinamide mononucleotide show mixed biochemical results across different study designs.
The landscape is growing but heterogeneous. Some trials report substantial rises in whole-blood nad levels after about 60 days at 600 mg/day. Other studies using similar doses report little or no change.
Key drivers of variability include dose, study length, participant age and health, and lab methods. Sample handling and the assay used to measure metabolites make a big difference.
What influences outcomes
- Design factors: dose, duration, and demographics affect results.
- Bioanalysis: extraction, storage, and assay choice change reported nad levels.
- Tissue differences: skeletal muscle responses are inconsistent, mirroring nicotinamide riboside findings.
- Formulation issues: stability, particle size, and crystalline form can alter absorption with oral supplementation.
Safety: Early signals show NMN is generally well tolerated in small trials among older adults. Larger, longer trials are needed for hard clinical endpoints.
For study methods and to compare trials, read original reports and trial protocols on clinical overviews and search details on google scholar. Future work should include head-to-head NR vs. NMN comparisons and standardized sampling to improve consistency.
NAD+ supplements vs. a multitarget approach: beyond single precursors
A systems-based strategy aims to nudge multiple control points in cellular metabolism rather than relying on a single precursor.
Why consider a multitarget design? Single agents like nicotinamide riboside or nicotinamide mononucleotide can raise circulating levels in many trials. But age-related changes in nad metabolism — higher consumption and weaker recycling — can blunt long-term gains.
Addressing root causes: NAMPT activation, CD38 inhibition, NNMT modulation
One way to relieve the salvage pathway bottleneck is to support nicotinamide phosphoribosyltransferase. Raising NAMPT may help sustain increasing nad by improving recycling.
Lowering CD38-driven consumption and reducing NNMT diversion are other logical targets. Together, these moves try to both boost synthesis and slow losses.
Early human signals: NAD+ increases, inflammatory cytokines, and glycation
A double-blind crossover trial of a systems-based product reported a 26.5% mean rise in whole-blood NAD (enzymatic assay). The same study found higher SIRT1 and NAMPT in PBMCs, lower pro-inflammatory cytokines (including IL-2), and reduced glycated serum proteins.
Safety and limits: Adverse effects were minimal, but the sample size was modest. Clinical outcomes such as blood pressure, mobility, or cognition were not primary endpoints and need larger trials and replication in npj aging and related journals.
How this compares to single-precursor use: Multitarget strategies are hypothesis-driven. They aim to complement or improve on nicotinamide riboside or nicotinamide mononucleotide by fixing age-related machinery issues rather than only adding substrate.
- Balance matters: chronic nicotinamide exposure needs monitoring in multitarget designs.
- Read methods carefully: assay choice and endpoints determine how convincing results are.
- Track new studies on google scholar to watch replication and larger trials.
| Strategy | What it targets | Early human signals |
|---|---|---|
| Single precursor (NR/NMN) | Supply: raises circulating precursor levels | Consistent blood gains; mixed tissue uptake |
| NAMPT activation | Recycling: improves salvage pathway throughput | Higher NAMPT protein in PBMCs; may support sustained increases |
| CD38 / NNMT modulation | Demand/diversion: lowers consumption, limits loss | Reduced inflammatory markers and improved glycation profile |
NAD+ supplements and skeletal muscle: focus on human skeletal muscle NAD
Skeletal muscle is a high-demand tissue with compartmentalized stores, making it a tough but important target for interventions that aim to change cellular cofactors.
Why muscle is challenging: Human skeletal muscle has large, localized pools and high metabolic flux. That compartmentalization can blunt measurable shifts in total muscle nad despite clear rises in blood markers.
Clinical trials illustrate this gap. In older men, three weeks of nicotinamide riboside (500 mg twice daily) raised NAAD and methylated nicotinamide metabolites in muscle without changing total muscle NAD+ or mitochondrial bioenergetics. Shorter, 7-day trials showed no change in skeletal muscle NAD+, mitochondrial function, or sirtuin activity at rest or after exercise.
These metabolite changes—NAAD rises and more methylated products—suggest pathway engagement even when bulk muscle nad stays static. They hint that the precursor reached tissue and underwent metabolism, but did not expand the steady-state pool measured by common assays.
- Interindividual variability is large; baseline fitness, diet, and recent activity shape responses.
- One crossover trial reported body composition shifts, but replication is needed before firm conclusions.
- Measurement issues—assay type, biopsy timing, and post-exercise sampling—can change results markedly.
Practical takeaways: Athletes and active older adults should set measured expectations. Short trials tend to show systemic marker rises more often than consistent muscle nad increases. Tissue-targeted dosing, longer interventions, or multitarget strategies may better move intramuscular pools.
Track upcoming muscle-focused trials and meta-analyses on google scholar to watch for standardized protocols, pooled effect sizes, and clearer guidance for skeletal muscle outcomes.
Liver health and NAD+: non-alcoholic fatty liver and fatty liver disease
Hepatic mitochondrial health depends on molecules that support fat burning and detox pathways.
Non-alcoholic fatty liver and broader fatty liver disease occur when metabolic stress and inflammation drive fat buildup in hepatocytes. That state links to insulin resistance, oxidative stress, and altered adenine dinucleotide balance in the liver.
NAD+, mitochondrial dysfunction, and metabolic pathways in the liver
Preclinical work shows that restoring nicotinamide adenine dinucleotide in liver cells boosts beta-oxidation and mitochondrial resilience. Improved cellular nad metabolism reduces lipotoxic stress and supports detox pathways.
Animal models report less steatosis, better mitochondrial respiration, and protection after injury. Human trials, however, rarely target NAFLD endpoints directly and remain early. Most studies focus on safety and systemic markers rather than imaging or biopsy outcomes.
Clinical implications: Lower cellular nad can worsen hepatic insulin resistance and oxidative damage, speeding steatosis progression. Systemic gains—better vascular tone or lower inflammatory cytokines—may indirectly ease liver burden. Improvements in skeletal muscle metabolism can also reduce hepatic fat over time.
For people with liver disease, prioritize medical care and lifestyle measures. Track emerging NAFLD trials and imaging or biopsy endpoints on google scholar to follow rigorous testing of this approach.
| Topic | Preclinical signal | Human evidence |
|---|---|---|
| Beta-oxidation | Increased with restored cofactor pools | Indirect markers; few direct NAFLD trials |
| Mitochondrial function | Improved respiration and resilience | Early systemic marker changes; limited liver endpoints |
| Clinical guidance | Promising mechanism | Use as adjunct; follow trials on google scholar |
NAD+ supplements and the brain: Alzheimer disease, oxidative stress, and cognition
Neurons demand constant energy and strong repair pathways, which makes the brain a logical focus for metabolic interventions.
Why the brain is a prime target: nicotinamide adenine dinucleotide supports neuronal ATP production, helps limit oxidative stress, and powers DNA repair enzymes that protect neurons from damage and degeneration.
Preclinical Alzheimer disease models show that restoring this cofactor improves memory, promotes nerve regeneration, and lowers markers of neurodegeneration. These animal studies link better mitochondrial function and sirtuin signaling to clearer cognitive gains.
Human data on cognition remain limited. Most clinical trials measure biochemical changes in blood or CSF rather than direct cognitive endpoints. That means early human signals are encouraging but preliminary.
Mechanistically, stronger sirtuin activity, reduced oxidative burden, and improved mitochondrial resilience could translate into brain protection if gains are sustained over time.
Tissue delivery is a key hurdle: crossing the blood–brain barrier and achieving therapeutic brain levels with oral dosing can be challenging. Both nicotinamide riboside and nicotinamide mononucleotide are under study for neuroprotective potential, but proof in people is still emerging.
- Systemic biology: lowering biological age markers and neuroinflammation may indirectly help brain health.
- Peripheral links: skeletal muscle metabolism and muscle nad influence whole-body metabolism and can affect brain resilience.
- Practical note: sleep, exercise, and vascular health remain foundational while research advances.
Watch for updates: check ongoing neuro-focused trials and reviews on google scholar to track cognitive outcomes and larger human studies.
Dosing and timing: how middle-aged and older adults are using NR and NMN
Dosing and timing decisions shape how reliably oral regimens change blood markers and, over time, tissues such as skeletal muscle.
Clinical dose ranges, trial durations, and tissue-specific responses
Typical clinical ranges: nicotinamide riboside trials most often test 100–1,000 mg/day (some up to 2,000 mg/day) over 2–20 weeks. Nicotinamide mononucleotide studies commonly use 250–600 mg/day for 6–12+ weeks.
Blood levels rise faster and show dose-response relationships in many trials. Changes in skeletal muscle usually lag and often require longer or targeted protocols to appear.
Oral supplementation bioavailability and formulation nuances
Formulation matters. Stability, particle size, and crystalline form can influence absorption and conversion. These factors help explain variable outcomes between trials and brands.
Consistency and timing also matter. Trials use morning dosing or split doses to keep levels steady, although no single schedule is standard yet.

- Start with study-aligned doses and monitor how you feel; avoid escalating beyond published ranges without medical input.
- Mononucleotide supplementation studies are growing; results vary with duration and lab methods.
- Nicotinamide riboside supplementation has the largest human evidence base, but head-to-head trials are limited.
- Older adults or those on medications should consult clinicians about interactions and dosing.
- Use google scholar to find pharmacokinetics and bioavailability papers for specific brands and formulations.
| Agent | Common clinical dose | Time to detectable blood change |
|---|---|---|
| nicotinamide riboside | 100–1,000 mg/day (up to 2,000 mg in some trials) | Weeks |
| nicotinamide mononucleotide | 250–600 mg/day | Several weeks to months |
| Muscle response | Variable | Often months or longer; assay dependent |
“Expect weeks to see blood changes and longer periods for tissue adaptations or clinical outcomes.”
Safety and side effects: what clinical trials report
Clinical trials to date paint a generally reassuring safety picture for oral nicotinamide riboside and related precursors, especially in older adults, but a few practical cautions matter.
Tolerability, lab markers, and potential blood pressure effects
Overall tolerability: Most controlled trials report few mild adverse events. Older adults in study cohorts tolerated study doses well, with only occasional complaints of sleep disturbance or mild stomach irritation.
Routine labs: Liver enzymes and common safety labs usually remain within normal limits during monitored trials. Serious lab abnormalities are rare in the published reports.
Cardiovascular signals: One trial showed exploratory reductions in blood pressure, but other studies did not replicate that effect. There is no consistent hypertensive or hypotensive risk signal identified so far.
Interactions, chronic nicotinamide exposure, and practical precautions
Chronic nicotinamide concerns: Long-term exposure raises questions about methylated metabolite load and excretion. Keeping pathways balanced matters to avoid excessive byproduct accumulation.
sirt1 activity: Some tissues show little consistent change in sirt1 activity over short trials, highlighting that biochemical shifts do not always equal functional change.
Who should be cautious: People on anticoagulants, those receiving chemotherapy, or individuals with active cancer should seek medical advice before use. Pregnancy, lactation, and pediatric safety data are limited.
Practical steps: Monitor for sleep or GI changes, adjust timing or dose if needed, and review full adverse event tables and lab data in full-text papers on google scholar rather than relying on abstracts.
| Safety area | Trial findings | Practical note |
|---|---|---|
| Tolerability | Mostly mild events (GI, sleep); rare serious events | Older adults tolerated study doses well |
| Lab markers | Liver enzymes and routine labs generally stable | Check labs during longer or higher-dose studies |
| Blood pressure | Exploratory reductions in one study; mixed elsewhere | Not a consistent effect; monitor if hypertensive |
| Long-term exposure | Potential for increased methylated metabolites | Balance pathways; watch renal excretion and methylation status |
| Drug interactions | Limited data; caution advised | Consult clinicians for anticoagulants, chemo, or active cancer |
Quality and sourcing: Choose products with third-party testing to reduce contamination risk. For deeper review of adverse events and lab data, read full articles and trial reports on google scholar to assess study design, sample size, and assay methods.
How to vet research and reviews: using Google Scholar and reputable journals
Look for clear methods describing dose, duration, and assay techniques before trusting conclusions.
Start with google scholar to locate primary trials, reviews, and meta-analyses. Use quotes for exact phrases (e.g., “nicotinamide riboside clinical trial”) and Boolean operators (AND, OR) to narrow results. Filter by year and sort by date to see the latest human work.
Next, scan high-quality journals such as npj aging and Cell Rep. for mechanistic and trial reports. Pull full texts when possible to inspect methods: dose, duration, assay type, and statistical power.
- Verify trial registration on ClinicalTrials.gov and match reported outcomes to registered primary endpoints.
- Assess risk of bias, funding, and conflicts of interest in the paper and disclosure sections.
- Compare multiple studies instead of relying on single positive reports and read supplemental files for raw figures and assay details.
| Step | What to check | Why it matters |
|---|---|---|
| Search | Use google scholar; quotes & Boolean | Find primary trials and reviews quickly |
| Journal check | Scan npj aging, Cell Rep. | High-quality methods and peer review |
| Trial registry | ClinicalTrials.gov matching | Prevents outcome switching |
“Trace citations forward and backward to map how evidence evolves.”
NAD+ supplements: choosing products and setting realistic expectations
Good product choice combines clear labeling, third-party verification, and claims that reflect published human data.
Quality checklist: look for clear dosing that matches trials, cGMP manufacturing, and third-party testing such as USP or NSF. Prefer brands that cite peer-reviewed human studies rather than marketing claims.
Practical guidance before you buy
Expect oral supplementation to often raise whole-blood nad levels but not to guarantee faster performance or disease reversal. Effects on blood pressure, liver disease, and skeletal muscle are mixed in human trials.
- Try one product for 8–12 weeks and track energy, sleep, resting heart rate, and step counts.
- Check doses used in trials on human studies and compare with the label.
- Stack with sleep, resistance training, and balanced nutrition for better odds of benefit.
“Choose evidence-aligned products and measure changes; don’t expect instant cures.”
| Selection factor | What to check | Why it matters |
|---|---|---|
| Label dose | Matches clinical ranges for nicotinamide riboside or nicotinamide mononucleotide | Ensures you test a dose with human safety data |
| Third-party testing | USP/NSF or independent certificate | Reduces contamination and verifies content |
| Evidence cited | Peer-reviewed human trials and transparent methods | Helps avoid overhyped claims on fatty liver or performance |
NAD+ supplements
Raising cellular cofactor levels in blood is often easier than turning that change into clearer improvements in strength or endurance.
Increasing NAD vs. improving outcomes: the role of context and baseline health
Increasing nad in whole blood is a repeatable finding in trials, especially with nicotinamide riboside. But a lab rise does not always translate to better muscle function or endurance.
Baseline health matters. Middle-aged older adults who are sedentary, insulin resistant, or nutrient‑deficient often respond differently than fit people who train regularly.
Think of the role nad plays as necessary but not sufficient. Pairing an increase nad strategy with resistance training, good protein intake, and sleep raises the odds of real gains.
Skeletal muscle responses can lag. Tissue uptake, assay methods, and duration affect whether cellular nad rises in muscle and whether function improves.
- Be patient and track performance, sleep, and labs over 8–12 weeks.
- If no change, review dose, timing, or try alternative formulations.
- Validate claims against peer‑reviewed trials on google scholar and discuss use with a clinician when on medications.
“Context and consistency often determine whether rising cellular nad turns into real-world benefits.”
Conclusion
Overall, trials show clear blood marker gains but leave open whether these biochemical shifts become lasting health benefits.,
Clinical data indicate increases in nad levels in blood with generally good tolerability. Small trials report promising drops in inflammation and mixed vascular signals, yet robust effects on biological age or function remain unproven.
Strong preclinical and in vivo nad work — including models relevant to alzheimer disease and conditions like ataxia telangiectasia — motivates larger, longer human trials.
For now, pair any use with proven habits: resistance training, sleep, and good diet. Track papers on google scholar, choose products and dosing carefully, and monitor labs with your clinician.
Thanks for reading. As study size and quality grow, we’ll better know when adenine dinucleotide strategies move from promising markers to meaningful health outcomes.
FAQ
What are nicotinamide riboside (NR) and nicotinamide mononucleotide (NMN) and how do they relate to nicotinamide adenine dinucleotide?
Both NR and NMN are precursors that the body can use to make nicotinamide adenine dinucleotide, a key cellular cofactor. They feed into biosynthesis and salvage pathways to help maintain intracellular levels that support mitochondrial function, sirtuin activity, and DNA repair. Researchers study NR and NMN in contexts such as healthy middle-aged adults, older adults, and conditions like non-alcoholic fatty liver disease.
Do oral NR or NMN increase tissue levels in humans, for example in skeletal muscle or liver?
Clinical trials report increases in blood and sometimes whole‑body measures, but changes in human skeletal muscle and liver are variable. Study factors such as dose, formulation, trial duration, baseline metabolic health, and analytical methods influence outcomes. Some trials show modest boosts in muscle NAD and improved mitochondrial markers, while others find little change.
What clinical benefits have been reported for cardiometabolic health and blood pressure?
Evidence is mixed. A few studies note modest improvements in vascular function or arterial stiffness and small blood pressure effects, but many trials show neutral cardiometabolic results. Larger, longer trials that measure inflammatory cytokines, glycation markers, and biological age proxies are needed to draw stronger conclusions.
Are NR and NMN safe for middle-aged and older adults? What side effects should be expected?
Short-term use in clinical trials is generally well tolerated with mild gastrointestinal symptoms reported occasionally. Lab markers remain stable in most studies. Concerns about chronic nicotinamide exposure and interactions with medications mean people with liver disease, ataxia telangiectasia, or on certain prescriptions should consult a clinician first.
How do NR and NMN differ in mechanism and clinical evidence?
NR converts to NMN and then to the active cofactor via the salvage pathways involving enzymes like nicotinamide phosphoribosyltransferase (NAMPT). NMN may enter cells via specific transport routes in some tissues. Clinical trials differ in dosing and outcomes: NR has more randomized human data on tolerability and blood NAD changes, while NMN trials show variable whole-blood responses and limited tissue data.
Can boosting cellular levels improve muscle function or reduce age‑related decline?
Animal models show promising effects on muscle function, mitochondrial biogenesis, and oxidative stress. Human data are preliminary: some small trials suggest improvements in muscle metabolism or markers of function in older adults, but results are not yet consistent across populations or endpoints.
What about liver disease, especially non‑alcoholic fatty liver disease (NAFLD)?
Preclinical studies indicate that restoring cofactor levels can improve mitochondrial function and metabolic pathways in the liver. Human evidence is emerging; a few early trials look at fatty liver outcomes and metabolic markers, but robust clinical proof in NAFLD patients is still limited.
Are there interactions with sirtuins, PARPs, CD38, or NNMT that matter clinically?
Yes. Sirtuins and PARPs consume the cofactor for key signaling and DNA repair processes, while CD38 and NNMT can lower available levels by increased breakdown or methylation pathways. Effective strategies may combine precursor use with approaches that target CD38 inhibition or NAMPT activation to address bottlenecks in biosynthesis.
How should someone evaluate research and product claims?
Use Google Scholar and reputable journals such as npj Aging and Cell Reports to read primary trials. Look for randomized, placebo‑controlled studies, clear tissue measurements, third‑party testing for product quality, and transparent dosing. Clinical trial registries can reveal ongoing studies and registered endpoints.
What dosing ranges and durations have clinical trials used for oral NR and NMN?
Trials vary, typically using daily doses from low hundreds of milligrams up to a gram or more, over weeks to months. Tissue responses and safety profiles depend on dose, formulation, and individual baseline health. Consult clinical data for specific regimens and a healthcare provider before starting.
Will raising cellular cofactor levels change my biological age or cognition, for example in Alzheimer disease?
Some biomarkers of biological age and preclinical brain studies show promise for reducing oxidative stress and supporting neuronal health. Clinical evidence for meaningful cognitive protection or reversal in Alzheimer disease remains preliminary and requires larger, longer trials focused on cognition and disease progression.
Should boosting levels be the only focus, or is a multitarget approach better?
A multitarget approach often makes more sense. Addressing root causes like inflammation, CD38 activity, NAMPT function, and metabolic health alongside precursor use gives a better chance of translating biochemical increases into meaningful clinical improvements.
