Have you ever woken to a face that felt puffy or a limb that felt heavy after a long week? That small, constant swelling can be frustrating and affect how you move, dress, and feel each day. I remember the first time I noticed my wrist ring fitting tight — it made me look for gentle ways to help my body balance itself again.
This guide explains what lymphatic drainage is and how gentle movements and light massage can help shift excess fluid so tissues feel lighter. You’ll learn when it helps conditions like lymphedema and when to check with a healthcare provider before trying techniques at home. Consider complementary approaches like functional wellness treatments or personalized IV therapy solutions for comprehensive health optimization.
For a reliable primer on the basics and medical context, see this short overview at lymphatic drainage massage. Read on and you’ll gain clear, safe steps to support your system with gentle care.
Key Takeaways
- Gentle, rhythmic movements can help move excess fluid and ease tightness.
- This approach can support people with swelling or lymphedema, but isn’t for everyone.
- Light massage feels soft on the skin and avoids deep compression.
- Always discuss new routines with your healthcare provider first.
- Practical at-home sequences and aftercare tips help maintain comfort and safety.
What lymphatic drainage therapy is and why it helps right now
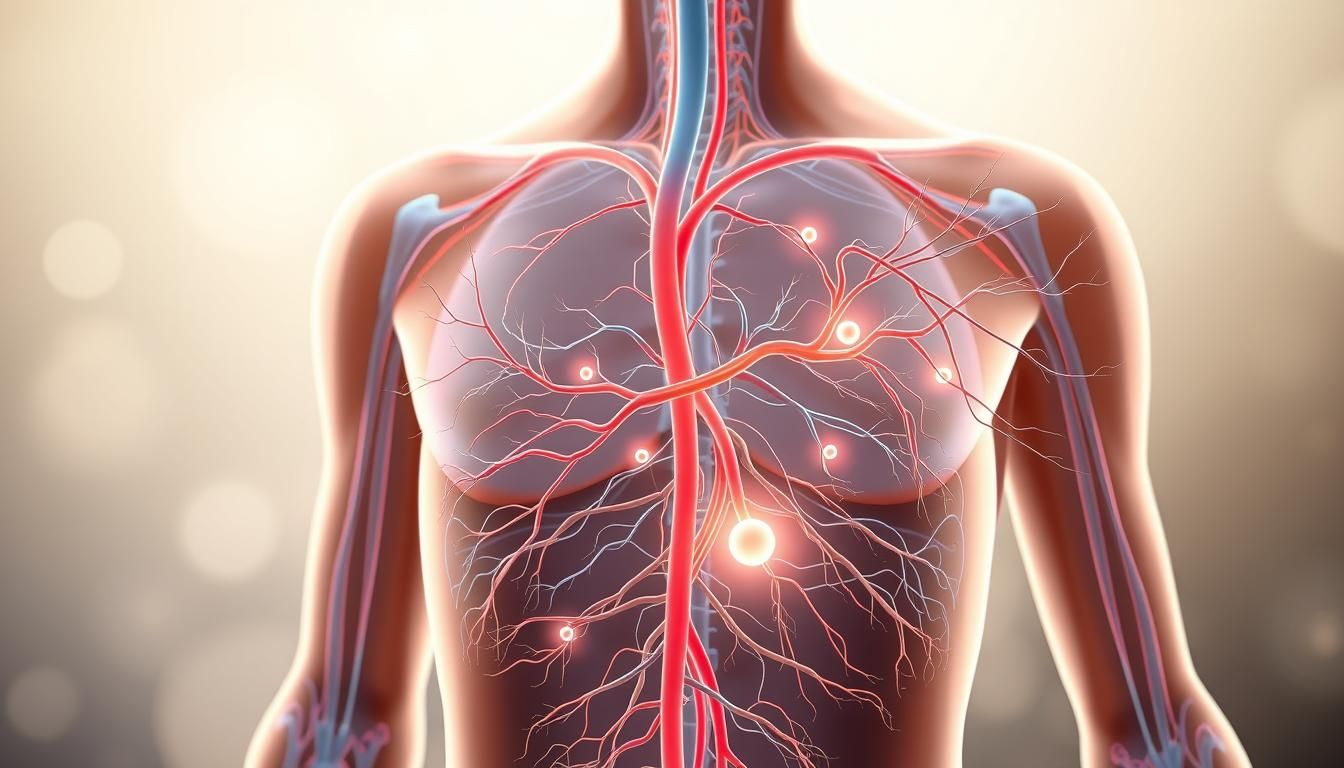
When flow slows in the body’s network of vessels, tissue can feel heavy and swollen. The system moves lymphatic fluid through vessels that connect lymph nodes. White blood cells in those nodes filter out debris and help fight infection.
Light, skin-focused techniques aim to guide fluid toward working nodes so congested areas can clear. People with lymphedema after node removal, surgery, or infection may see less swelling and better range of motion when these methods are used as part of care.
How the system works
The vessels carry lymph and let immune cells monitor the body. When flow stalls, fluid builds in an area and causes the swelling known as lymphedema.
Benefits and who may gain
Benefits include reduced swelling, improved comfort, and easier movement. A 2021 review also suggested people with fibromyalgia might notice quality-of-life gains from gentle massage.
Indications include post-surgical buildup, vascular procedures, infection-related swelling, trauma, or DVT-associated edema. Always check with a clinician before starting techniques at home.
| Condition | Why it helps | Typical outcome |
|---|---|---|
| Post-surgical swelling | Redirects fluid toward intact nodes | Less tightness, improved motion |
| Lymphedema after node removal | Encourages alternate vessel pathways | Reduced buildup with supervision |
| Fibromyalgia (adjunct) | May ease discomfort and improve well-being | Quality-of-life improvements reported |
For a detailed overview of how these methods fit into broader care, see this summary. Start with education on the correct area and gentle pressure to reduce risk and improve results.
Safety first: who should avoid lymphatic drainage and how to prepare
Start with a quick safety check so you can protect your health and get benefits without harm.
Contraindications and when to talk to a healthcare provider
Do not perform massage if you have active infection, unexplained fever, cellulitis, blood clots or DVT, cancerous tissue, radiation‑damaged skin, tuberculosis, or certain heart or kidney conditions. Talk to your healthcare team before trying any technique if you are recovering from illness or on new medications.
“If in doubt, pause and consult a clinician—safety beats speed when it comes to managing fluid and sensitive areas.”
Pressure, pace, and what “gentle” really means for skin and vessels
Gentle pressure means skin-only contact. Use feather-light strokes that move the surface without pressing into muscle. You should feel a soft stretch, not pain, redness, or bruising.
Prep steps: deep lymphatic breathing and node activation
Begin with diaphragmatic breathing: hands on ribs, inhale into the belly, exhale slowly. This helps move lymphatic fluid with no strain.
Prime nodes with 10–15 light pumps at the front and back of the neck, under the arms, and behind each knee before working limbs.

Hydration, compression, and skin care considerations
Hydrate after a session to support fluid shifts. People with chronic swelling often combine massage with compression garments, gentle exercise, and daily skin care to prevent infection.
Stop and contact healthcare support for sudden pain, dizziness, or increased swelling.
| Situation | Why avoid | Action |
|---|---|---|
| Blood clots / DVT | Risk of dislodging a clot into circulation | Contact healthcare; no massage until cleared |
| Active infection or cellulitis | May spread infection locally or systemically | Delay until infection is treated |
| Radiation-damaged or cancer-treated skin | Fragile tissue, altered vessel function | Avoid massaging treated area; consult oncology team |
How to perform lymphatic drainage therapy at home
Begin by calming the body with five slow breaths, hands on the ribs. This primes breathing to move fluid and steady the heart rate.
Neck and chest priming: place index and middle fingers below each earlobe and slide the skin toward the shoulders 10–15 times. Turn palms near the hairline and glide down the back of the neck 10–15 times. Cup each armpit with a hand and make small upward pumps to activate axillary lymph nodes.

Upper and lower body sequence
For the chest and shoulder, sweep the opposite chest over the collarbone and up the neck. Use a gentle motion on the back of the shoulder toward the neck. On the arm, start at the shoulder and use upward skin stretches down to the wrist.
At the wrist and fingers, use light strokes from fingertip toward the hand and forearm. For the leg, one hand at the inner thigh near the groin and the other on the buttock. Step down the thigh, stopping above the knee, then stretch the lower leg upward toward the ankle. Finish toes with light strokes tip to base.
Facial flow, finishing moves, and aftercare
Activate chest and repeat gentle neck downstrokes. Use soft circles above the brows toward the temples and light undereye sweeps to the chest. Finish by sweeping from the center of the chest to each armpit about ten times, then repeat neck slides.
Aftercare: drink water and rest. Mild tiredness or a brief headache can occur as excess fluid shifts. If swelling or pain increases, stop and consult your clinician.
| Step | Area | Key action |
|---|---|---|
| Prime breathing | Chest | Five deep breaths, hands on ribs |
| Neck slides | Front & back neck | 10–15 gentle slides toward shoulders/spine |
| Arm strokes | Shoulder to wrist | Upward skin stretches, light pressure |
| Leg sequence | Thigh to toes | Inner thigh lift, lower leg upward strokes |
| Finish | Chest & armpits | Sweep center chest to each armpit ~10 times |
When to see a massage therapist and how to build a routine
When swelling hangs on or home methods leave questions, it’s time to bring in a trained massage therapist. A skilled practitioner assesses your condition and teaches safe steps you can repeat at home.
Manual care vs. simple self-care
Manual lymphatic massage is done by a certified therapist who tailors pressure, sequence, and targets affected nodes. This work may use precise moves that a person cannot replicate alone.
Simple self-drainage refers to the lighter techniques a therapist can teach so people maintain gains between visits.
Frequency, compression, and decongestive plans
Decongestive lymphatic therapy (DLT) blends massage, skin care, exercise, and compression garments. Early phases often require daily sessions for several weeks, then fewer visits as progress stabilizes.
- See a massage therapist when swelling is persistent, or techniques feel confusing.
- A therapist can train you in self-care and proper pressure to avoid harm.
- People with prior DVT or heart issues must coordinate with healthcare before intense sessions; blood flow and pressure need monitoring.
| Need | What a therapist provides | Typical times |
|---|---|---|
| New or worsening lymphedema | Assessment, tailored manual work, education | Daily to several times weekly |
| Maintenance | Self-drainage skills and compression guidance | Weekly or as needed |
| Complex post-surgical changes | Integrated DLT plan with exercise and skin care | Initial frequent visits then taper |
“Regular check-ins and simple progress markers—tape measures, photos, or fit of clothing—help you and your therapist track results.”
Build a routine by matching session length to your schedule, using light touch daily at set times, and revisiting professional care when goals or symptoms change.
Conclusion
Conclude with gentle, skin-level motion aimed at the nodes you primed at the start. Move the skin—not the muscle—and guide flow slowly toward the chest and neck.
A few minutes each day can ease swelling, improve motion, and help your body feel lighter. Hydrate afterward and rest if you feel tired.
If progress stalls or you have medical conditions, seek a trained therapist who can add compression, skin care, and tailored manual work. Learn more about lymphatic drainage massage benefits to pair home routines with professional support.
FAQ
What is lymphatic drainage therapy and why try it now?
Lymphatic drainage therapy is a gentle hands-on approach that helps move excess fluid and support immune function. It uses light, rhythmic strokes to encourage flow through vessels and nodes, which can reduce swelling and improve comfort. People choose it now for post-surgical recovery, ongoing swelling like lymphedema, or to boost a wellness routine.
How does the system move fluid, toxins, and support immunity?
The network of vessels and nodes collects fluid, proteins, and waste from tissues and returns them to the bloodstream. Manual work and specific breathing techniques help open pathways and move fluid toward central nodes, supporting the removal of cellular waste and aiding immune cells in surveillance.
What benefits can I expect for swelling, lymphedema, and overall well-being?
Benefits include reduced puffiness, improved range of motion, less heaviness in affected areas, and a calmer nervous system. For those with mild to moderate swelling or early-stage lymphedema, regular sessions—combined with compression and exercise—often yield the best results.
Who may benefit based on current evidence?
People recovering from certain surgeries, those with chronic mild swelling, and individuals seeking gentle support for immune and circulatory health often benefit. Always consult a clinician for complex medical conditions like active infections, deep vein thrombosis, or severe heart failure.
Who should avoid this work and when should I talk to a healthcare provider?
Avoid treatment if you have an untreated infection, uncontrolled congestive heart failure, active blood clots, or recent cancer treatments without medical clearance. Speak with your doctor before starting if you have vascular disease, kidney problems, or any acute illness.
What does “gentle” mean for pressure, pace, and skin and vessel safety?
Gentle means light, superficial strokes that stretch the skin without deep kneading. The pace is slow and repetitive to stimulate superficial vessels without compressing deeper structures. Trained hands monitor skin color and response to avoid irritation or bruising.
How should I prepare—breathing, node activation, and skin care?
Begin with deep diaphragmatic breathing to create pressure changes that favor flow. Activate central nodes at the neck and chest with light strokes before working limbs. Keep skin clean, hydrated, and free of wounds; remove tight jewelry or clothing.
What about hydration, compression, and post-care for the skin?
Drink water before and after sessions to aid fluid movement. Compression garments may be recommended after sessions for chronic swelling. Apply gentle moisturizer to soothe skin; avoid hot baths or intense exercise right away if treatment was vigorous.
How do I perform a safe home routine for the neck and chest priming?
Start by lightly stroking the base of the neck and upper chest in a one-way direction toward the collarbone to clear central nodes. Use soft, repetitive motions with just enough pressure to move the skin, repeating each stroke several times to prime the area.
What sequence should I use for the upper body: chest, shoulder, arm, wrist, fingers?
After priming, move from the chest to the shoulder, then stroke down the arm toward the axilla. Work the wrist and fingers with gentle pumps and sweeping motions back toward the armpit nodes. Repeat each area 5–10 times, keeping motions slow and light.
What about lower body sequence: thigh, calf, ankle, toes?
Begin by clearing the groin nodes, then sweep from the upper thigh down toward the knee and calf, finishing at the ankle and toes. Always direct motion toward the nearest working node and use repeated, gentle strokes rather than deep pressure.
How do I do a gentle facial flow for forehead, under-eye, and neck?
Use very light fingertip strokes from the center of the forehead outward, then sweep under the eyes toward the ears and down the neck to the collarbone. Keep movements feather-light and limit repetitions to avoid irritation of delicate facial skin.
What are finishing moves and how do I return flow toward axillary and neck nodes?
Finish with broad, gentle strokes from the limbs toward the trunk and light pumps over the axillary and neck nodes to encourage final clearing. Re-activate central nodes at the collarbone to help fluids re-enter circulation.
What aftercare should I follow—water, rest, and normal sensations?
After a session, drink water, rest briefly, and expect mild warmth, tingling, or increased urination as fluid shifts. Soreness or bruising is not normal; if you feel pain, seek professional advice. Continue gentle movement and follow any garment or exercise guidance from your provider.
When should I see a massage therapist instead of self-care?
See a trained therapist if you have persistent swelling, post-surgical needs, or complex conditions like advanced lymphedema. Professionals can assess, apply certified techniques, and coordinate care such as compression bandaging and decongestive strategies.
What’s the difference between manual therapy by a therapist and simple self-drainage?
A therapist is trained to assess tissue, node function, and identify contraindications. They can use advanced sequences and adjuncts like compression. Self-drainage teaches basic strokes for daily maintenance, but it cannot replace clinical assessment for serious conditions.
How often should sessions occur, and when are compression garments recommended?
Frequency depends on goals: acute care may need several sessions per week, while maintenance often works with once-weekly or biweekly visits plus daily self-care. Compression garments are commonly used for chronic swelling and should fit under professional guidance.